The Process of Dying
Learning Outcomes
- Explain physiological death
- Describe social and psychological death
Aspects of Death
One way to understand death and dying is to look more closely at physiological death, social death, and psychological death. These deaths do not occur simultaneously, nor do they always occur in a set order. Rather, a person’s physiological, social, and psychological deaths can occur at different times.[1]
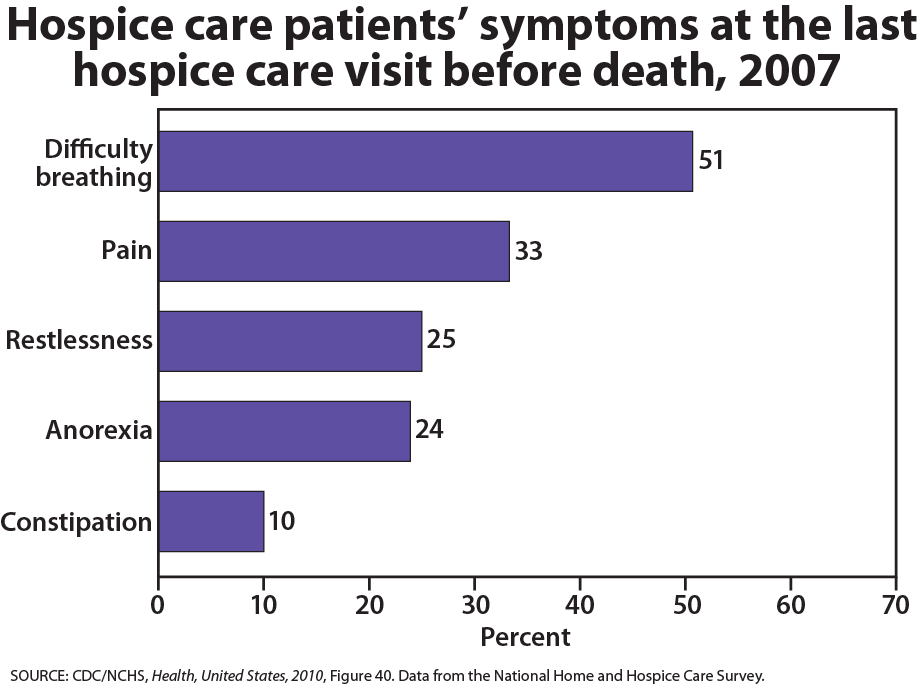
Physiological death occurs when the vital organs no longer function. The digestive and respiratory systems begin to shut down during the gradual process of dying. A dying person no longer wants to eat as digestion slows, the digestive track loses moisture, and chewing, swallowing, and elimination become painful processes. Circulation slows and mottling, or the pooling of blood, may be noticeable on the underside of the body, appearing much like bruising. Breathing becomes more sporadic and shallow and may make a rattling sound as air travels through mucus- filled passageways. Agonal breathing refers to gasping, labored breaths caused by an abnormal pattern of brainstem reflex. The person often sleeps more and more and may talk less, although they may continue to hear. The kinds of symptoms noted prior to death in patients under hospice care (care focused on helping patients die as comfortably as possible) are noted below.
When a person is brain dead, or no longer has brain activity, they are clinically dead. Physiological death may take 72 or fewer hours. This is different than a vegetative state, which occurs when the cerebral cortex no longer registers electrical activity but the brain stems continues to be active. Individuals who are kept alive through life support may be classified this way.
Watch it
This video explains the difference between a vegetative state, a coma, and being brain dead.
You can view the transcript for “Is A Brain Dead Person Actually Dead?” here (opens in new window).
Social death begins much earlier than physiological death. Social death occurs when others begin to withdraw from someone who is terminally ill or has been diagnosed with a terminal illness. Those diagnosed with conditions such as AIDS or cancer may find that friends, family members, and even health care professionals begin to say less and visit less frequently. Meaningful discussions may be replaced with comments about the weather or other topics of light conversation. Doctors may spend less time with patients after their prognosis becomes poor. Why do others begin to withdraw? Friends and family members may feel that they do not know what to say or that they can offer no solutions to relieve suffering. They withdraw to protect themselves against feeling inadequate or from having to face the reality of death. Health professionals, trained to heal, may also feel inadequate and uncomfortable facing decline and death. A patient who is dying may be referred to as “circling the drain,” meaning that they are approaching death. People in nursing homes may live as socially dead for years with no one visiting or calling. Social support is important for quality of life and those who experience social death are deprived from the benefits that come from loving interaction with others.
Psychological death occurs when the dying person begins to accept death and to withdraw from others and regress into the self. This can take place long before physiological death (or even social death if others are still supporting and visiting the dying person) and can even bring physiological death closer. People have some control over the timing of their death and can hold on until after important occasions or die quickly after having lost someone important to them. In some cases, individuals can give up their will to live. This is often at least partially attributable to a lost sense of identity. [2] The individual feels consumed by the reality of making final decisions, planning for loved ones—especially children, and coping with the process of their own physical death.
Interventions based on the idea of self-empowerment enable patients and families to identify and ultimately achieve their own goals of care, thus producing a sense of empowerment. Self-empowerment for terminally ill individuals has been associated with a perceived ability to manage and control things such as medical actions, changing life roles, and psychological impacts of the illness. [3]
Treatment plans that are able to incorporate a sense of control and autonomy into the dying individual’s daily life have been found to be particularly effective in regards to general attitude as well as depression level. For example, it has been found that when dying individuals are encouraged to recall situations from their lives in which they were active decision makers, explored various options, and took action, they tend to have better mental health than those who focus on themselves as victims. Similarly, there are several theories of coping that suggest active coping (seeking information, working to solve problems) produces more positive outcomes than passive coping (characterized by avoidance and distraction). Although each situation is unique and depends at least partially on the individual’s developmental stage, the general consensus is that it is important for caregivers to foster a supportive environment and partnership with the dying individual, which promotes a sense of independence, control, and self-respect.
Try It
https://assess.lumenlearning.com/practice/5a196f41-9ceb-4286-aa8d-ddb662721f42
https://assess.lumenlearning.com/practice/48cbc860-90f6-4de5-b4dd-b931298309df
https://assess.lumenlearning.com/practice/ef7dbc52-d5b6-4dc2-84e6-dfa2341c148a
Glossary
[glossary-page]
[glossary-term]active coping:[/glossary-term]
[glossary-definition]seeking information, working to solve problems; tends to produce more positive outcomes than passive coping[/glossary-definition]
[glossary-term]agonal breathing:[/glossary-term]
[glossary-definition]gasping, labored breaths caused by an abnormal pattern of brainstem reflex[/glossary-definition]
[glossary-term]brain dead:[/glossary-term]
[glossary-definition]when all brain function ceases to occur[/glossary-definition]
[glossary-term]clinical death:[/glossary-term]
[glossary-definition]when the individual is brain dead[/glossary-definition]
[glossary-term]passive coping:[/glossary-term]
[glossary-definition]characterized by avoidance and distraction; outcomes tend not be as positive as with active coping[/glossary-definition]
[glossary-term]physiological death:[/glossary-term]
[glossary-definition]when vital organs no longer function[/glossary-definition]
[glossary-term]psychological death:[/glossary-term]
[glossary-definition]when a dying person begins to accept death and to withdraw from others and regress into the self[/glossary-definition]
[glossary-term]social death:[/glossary-term]
[glossary-definition]when others begin to withdraw from someone who is terminally ill or has been diagnosed with a terminal illness[/glossary-definition]
[glossary-term]vegetative state:[/glossary-term]
[glossary-definition]the cerebral cortex no longer registers electrical activity but the brain stem continues to be active[/glossary-definition]
[/glossary-page]

